Here is a comprehensive list of the most common ocular conditions we come across, such as floaters, glaucoma, cataract, squint, retinal tear and detachment, conjunctivitis, retinopathy and cornea ulcer.
If you have any of these conditions, please contact us at 6733 5188 to make an appointment for us to have a look at your eyes.
Chalazion

This is caused by blockage of the oil secreting glands of the eyelid that is responsible for the oily component of our tear film. Chalazions are firm, mobile and usually painless swellings located a distance away from the lid margin.
Entropion / Ectropion
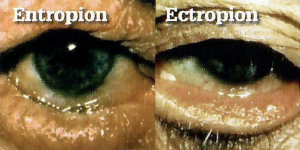
This occurs when the margin of the eyelid is turned in to cause the eyelashes to rub against the eye. Symptoms are redness, irritation, and tearing of the eye. In more sever cases, cornea abrasion and ulcer may result. Ectropion is the opposite condition of entropion, where the eyelid margin turns outwards.
Giant Papillary Conjunctivitis

GPC is a more severe type of allergic conjunctivitis that commonly occurs in contact lens wearers or atopic individuals i.e. those prone to suffer from allergic skin disorders, running nose, or asthma. Recurrent attacks are common.
Sub-Conjunctiva Haemorrhage
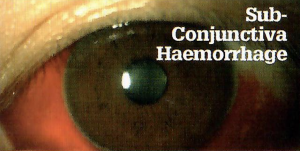
This appears as a localised red patch at the white of the eye. It is caused by rupture and bleeding of the fine capillary vessels of the conjunctiva. This painless condition often occurs spontaneously. No active treatment is required, and the blood will usually clear after 2 weeks.
Blepharitis

A common but often unrecognised condition characterised by chronic inflammation of the eyelid margins. Symptoms are itching, irritation and tearing. The eyelid margins are red and swollen with scaly dandruff present at the roots of the eyelashes.
External Hordeolum / Stye

Oftentimes confused with chalazion, this is an acute, pyogenic infection of an eyelash follicle and its attached oil gland. It begins as a tender, inflamed swelling at the eyelid margin but can enlarge to become a pointing abscess that may burst with release of yellow pus.
Pterygium
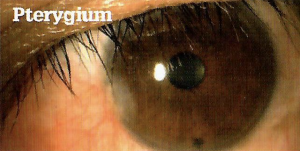
A fleshy, wing-shaped abnormal thickening of the conjunctiva adjacent to the cornea. Thought to be related to excessive exposure to the sun, When advanced, it will begin to encroach onto the clear cornea, causing astigmatism and even vision obstruction.
Cornea Ulcer
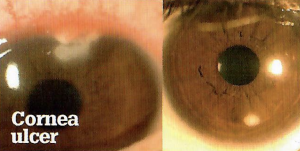
Ulcerative keratopathy is a feared complication of contact lens wear of cornea trauma. There is local necrosis of corneal tissue due to invasion by bacteria, fungi, viruses, or acanthamoeba. The eye is painful and red and a grey white opacity is noticed on the normally clear cornea.
Pinguecula
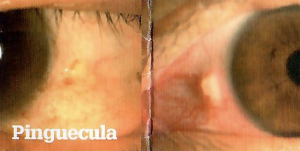
Often found in both eyes, it occurs as a small yellow-grey swelling located to the side of the cornea. It is caused by degeneration of the collagen fibres of the conjunctiva stroma with thinning of the overlying epithelium. Patients may complain of frequently red eyes and irritation.
Squint
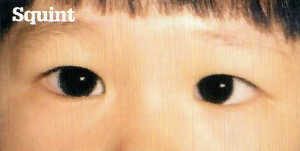
The medical name is strabismus. When a squint is present, the eyes are misaligned and point towards different directions. Esotropia or convergent squint is when the eye turns towards the nose bridge as opposed to exotropia or divergent squint.
Hyphaema
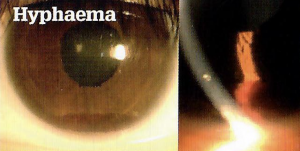
Blood in the anterior chamber of the eye. Usually caused by blunt trauma. With gravity, the blood pools inferiorly and a hyphaema level is observed. Mild to moderate hyphaema are best left alone to resolve spontaneously. It is important to watch for glaucoma that an be primarily from red blood cells clogging the drainage system or secondary from damage to the drainage structures.
Phlyctenular Kerato-Conjunctivitis
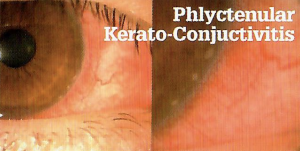
This is characterised by a history of recurrent localised conjuctiva inflammation and adjacent whitish peripheral cornea nodules. The patient typically presents with recurrent attacks of pain and redness. The underlying cause is a Type IV hypersensitivity reaction to bacterial and viral antigens or toxins.
Infective Conjunctivitis
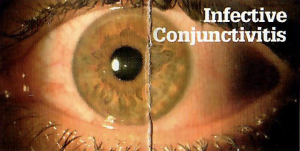
Bacteria infection is associated with pus-like discharges whereas virus infection causes watery discharges. May be highly contagious and one or both eyes may be affected. A good treatment strategy is to cover with both antibiotic eye drops and acyclovir eye ointment.
Herpetic Dendritic Keratitis
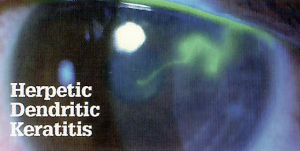
Typical history is that of a conjunctivitis that flares up to involve the cornea when steroid eye drops are added to the treatment regime. Fluorescein straining will show up a characteristic branching pattern of epithelial defects. The herpes simplex virus is never completely eradicated and recurrent attacks can occur.
Cataract
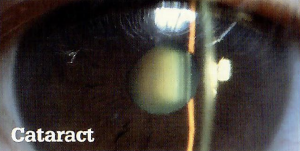
A cataract is a clouding of the normally clear crystalline lens of the eye. The most common cause is age-related but they can also occur from eye injury, taking certain medications, hereditary factors or foetal injection with viruses such as rubella. Treatment is surgical removal and replacement with an intraocular lens implant.
Iritis

This is an inflammation of the internal eye structures. Complaints are pain, redness, blurry vision, photophobia and tearing. The redness is more pronounced around the cornea (ciliary flush). Pupil reflexes may be sluggish and the pupil miosed (constricted).
Diabetic Retinopathy

Diabetes damages the small caliber retina blood vessels causing them to leak blood and fluid. Advanced diabetic eye disease causes hypoxia and proliferation of abnormal new retinal vessels that bleed and cause extensive retina damage and scarring. The risk of diabetic retinopathy is high when diabetes is present for many years. Blindness can be prevented by retinal laser therapy.
Papilledema from Malignant Hypertension
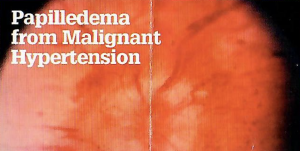
This condition must be suspected whenever a hypertensive patient complains of headache and blurry vision in both eyes. BP check finds severe hypertension. Fundoscopy reveals swollen optic discs and other features of hypertensive retinopathy such as flame haemorrhages, hard exudates and cotton wool spots.
Age-related Macular Degeneration (AMD)
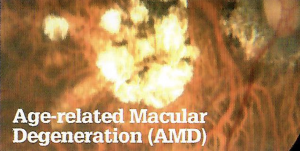
There are two types of AMD – dry and wet. Dry has a much better prognosis. Wet AMD can cause sudden devastating loss of central vision. Preventive measures include not smoking, eating fruits and vegetables, taking multi-vitamins and anti-oxidant supplements, avoiding strong sunlight, regular Amsler Chart monitoring and regular eye checks.
Central / Branch Retinal Vein Occlusion
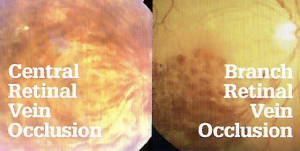
These conditions occur when the flow of blood through the retinal veins gets obstructed due to compressive forces at the site of the arteriole-venous crossings. Check for risk factors such as glaucoma, hypertension, diabetes, hyperlipidaemia, smoking and obesity.
Central Retinal Artery Occlusion (CRAO)
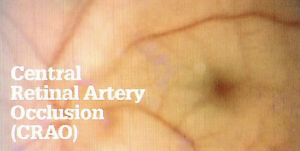
The main artery supplying oxygen rich blood to the retina can get blocked by emboli thrown off by other parts of the body. The complaint is of sudden, painless loss of vision in the affected eye. Fundoscopy will reveal a cherry red dot appearance of the macula against the pale retina. Refer immediately to an eye doctor for emergency eye treatment.
Optical Coherence Tomography (OCT)
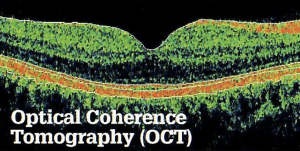
A recently developed equipment that scans the retinal non-invasively with laser light to give high-resolution two dimensional and even three-dimensional cross-sectional images of the retina. The OCT has helped clinicians to elucidate the pathology of many retinal disorders. The OCT is also able to evaluate the optic disc and nerve fibre layer that is helpful in glaucoma evaluation and management.
Central Serous Retinopathy
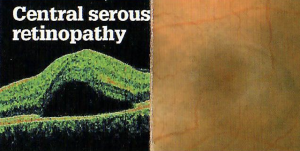
A common cause of central vision loss in young to middle age adults. The retinal pigment epithelium becomes leaky and there occurs a serous detachment of the overlying retina causing a relative central scotoma can be picked up with the Amsler grid test. The condition usually resolves spontaneously within three months.
Tonometry
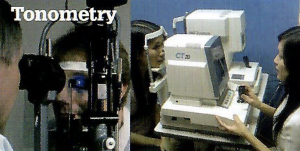
This is a test of the intra-ocular pressure (IOP) that is important in glaucoma diagnosis and management. The IOP shows diurnal variation with a range of 10mm to 21mm Hg (mean 14). It is most commonly performed using the automated air-puff tonometer or the Goldman applanation tonometer. The newly developed Pascal tonometer can measure the IOP accurately in patients who have had LASIK.
Visual Field Damage in Glaucoma

Glaucoma exacts its damage on the eye by means of a relative elevation of intra-ocular pressure in susceptible patients that in turn damages the optic disc nerve fibres. The visual loss starts from the peripheral visual fields. Hence the patient will usually not notice the visual loss until it encroaches upon the central vision by which time the patient would have suffered from irreversible tunnel vision. Hence chronic glaucoma comes on silently and is often called “the sneak thief of sight”.
Angle-Closure Glaucoma (ACG)
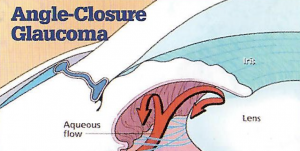
Glaucoma is known as the “sneak thief of sight”. ACG is associated with a closed or narrow anterior chamber drainage angles that result in increased intra-ocular pressures damaging the optic nerve. It is the more commonly seen glaucoma in Asian eyes as opposed to open angle glaucoma that is more commonly seen in Caucasian eyes.
Iridotomy for Angle Closure Glaucoma
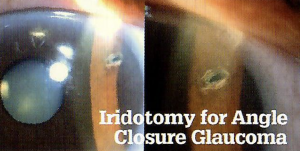
In eyes with narrow or closed anterior chamber angles, a channel can be artificially created at the root of the iris (iridotomy). This allows the aqueous humour produced by the ciliary processes behind the iris to short-cut its way out to the drainage channels at the angle of the eye without going through the pupil. In Asian eyes, iridotomy can be safely and effectively performed using “Sequential Argo-Yag laser iridotomy” – a procedure that is pioneered by Dr. Tony Ho.
Optic Disc Cupping
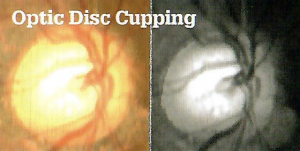
During fundoscopy, the normal optic disc has a central “cup” whose diameter is normally small in comparison to the optic disc diameter. The normal “cup-to-disc” ratio is 0.4 and should not exceed 0.6. In eyes with advanced glaucoma the cup-to-disc ratio exceeds 0.6, signifying significant loss of retinal nerve fibres. Eyes with tunnel vision have large deep cups of 0.8 to 0.9. At 1.0 there is total optic atrophy.
Floaters

This is the phenomenon of seeing fine wavy lines, dots, spots, cobwebs, mosquitoes or flies in front of the eyes. They seem to float in midair and follow the gaze of the eyes. They are most noticeable under certain lighting conditions. There are “benign” and “sinister” floaters. Benign floaters are usually few in number and have been there a long time. Sinister floaters are of sudden onset and come as a shower, and may be associated with seeing light flashes.
Retinal Tear and Detachment
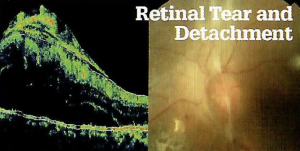
Complaints of sinister floaters usually precede a retinal tear. If the tear is left untreated, it may progress on to retinal detachment, where the neural retinal layer separates from its underlying retinal pigment epithelium. As the retina detaches, there is corresponding complaint of a shadow or curtain blocking the field of vision. Risk factors are high myopia, Marfan’s syndrome, trauma, positive family history, and history of a previous cataract operation.