1.What are cataracts? A cataract is essentially a clouding or loss of clarity of the clear crystalline lens of the eye. Cataracts are common as we age. It can be said that all of us will develop cataracts sooner or later in our life. Unsurprisingly, cataract surgery is one of the most common procedures performed…

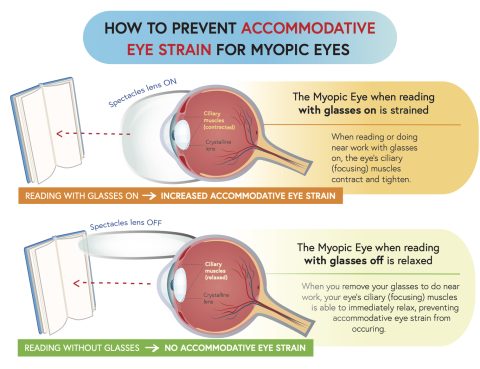
Childhood myopia management goes beyond spectacles and contact lenses! Usually after getting spectacles prescribed for their child, many parents are lulled into a sense of false complacency, thinking they have effectively managed the problem and do not need to take any further action. However, relying on spectacles or contact lenses without practicing good eye care…

Here is a comprehensive list of the most common ocular conditions we come across, such as floaters, glaucoma, cataract, squint, retinal tear and detachment, conjunctivitis, retinopathy and cornea ulcer. If you have any of these conditions, please contact us at 6733 5188 to make an appointment for us to have a look at your eyes….