1.What are cataracts?
A cataract is essentially a clouding or loss of clarity of the clear crystalline lens of the eye. Cataracts are common as we age. It can be said that all of us will develop cataracts sooner or later in our life. Unsurprisingly, cataract surgery is one of the most common procedures performed throughout the world. If you are diagnosed with cataract, rest assured – a cataract is not a tumour or growth in the eye.
2. What causes cataracts?
The most common cause of cataract is aging. But there are other causes. In infants, a cataract may be caused by infection, chemical imbalance, or developmental abnormality. Hereditary factors may also play a role in the development of cataracts. Diabetes and taking certain long-term medications such as steroids can also speed up development of cataract. Other causes include injury to the eye, excessive exposure to sunlight, smoking and extreme myopia.
3. What can one do to reduce the risk of cataracts?
With the damage to the earth’s ozone layer, we can expect more cataracts to develop as a result of the increasingly excessive exposure to ultra-violet rays. Thus one should wear good quality sunglasses when outdoors to protect their eyes from ultra-violet rays. While not scientifically proven, it may be wise to consider daily intakes of anti-aging antioxidant supplements. This should include the vitamins A (beta-carotene), C and E. Also, do not smoke. If you suffer from diabetes; visit your doctor regularly and strive to maintain good control of your blood sugar levels. If you are on steroid medications, you should discuss with your doctor about non-steroidal alternatives.
4. What types of cataracts are there?
The normal human crystalline lens is made up of layers of transparent cells enclosed within a clear lens capsule. The cataract or lens clouding can occur in any part of the human crystalline lens or affect the entire lens uniformly.
Cataracts are commonly classified as follows:
Polar cataracts: Here the clouding occurs at the front central or back central parts of the lens. They tend to affect younger patients who may have a history of taking long-term steroid medications. Posterior polar cataracts often adhere to the lens capsule and their removal may be complicated by the rupture of the lens capsule. In younger patients, these cataracts are best removed under general anaesthesia for the safest surgical outcome.
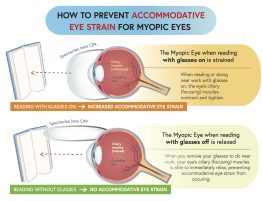
Nuclear cataracts: Here the whole lens undergoes widespread degenerative aging changes, causing it to harden and turn yellow-brown. This is the most common type of cataract. It will usually cause focusing problems, and frequent changes of spectacles lenses are needed. Those at risk of developing this type of cataract early are typically those who suffer from high myopia and those who spend long hours in the sun. Myopic patients with an onset of nuclear cataracts will often notice a sudden worsening of myopia power.
Coronary, sutural and cortical cataracts: Here the opacities usually start in the lens periphery. Vision is usually not badly affected unless the clouding progresses to affect the central parts of the lens.
5. What are the cataract symptoms?
The main complaint of a person with cataracts is blurred vision. In early cataracts, the blurred vision is often described as worse under strong sunlight or when the light is bright or when reading. Glare is another common complaint, especially when driving at night. As the cataract matures, the vision gets more and more blurred and colours appear less strong. In some early cataracts, vision may be improved slightly with corrective lenses. As the cataract matures, frequent changes of glasses are necessary and at some point, lenses will not help anymore.
The typical symptom of cataract formation is a slow, progressive, and painless decrease in vision. Other changes include: blurring of vision; glare, particularly at night; frequent eyeglass prescription change; a decrease in colour intensity; a yellowing of images; and in rare cases, double vision.
Ironically as the lens gets harder, farsighted or hyperopic people experience improved distance vision and are less dependent on glasses. However, nearsighted or myopic people become more nearsighted or myopic, causing distance vision to be worse. Some types of cataracts affect distance vision more than reading vision. Others affect reading vision more than distance vision.
6. Can cataracts cause pain?
Patients with cataracts sometimes complain of non-specific eyestrain symptoms, and these may sometimes be interpreted as eye pain. But there is a condition known as “acute lens (cataract) induced glaucoma” where the cataract causes sudden and severe pain accompanied by sudden and severe loss of vision. This is a medical emergency and treatment by an eye specialist should be sought as quickly as possible.
7. How are cataracts diagnosed?
Your eye doctor (ophthalmologist) is the best person to detect a cataract. A cataract is suspected in any person over the age of fifty who is unable to see clearly for distance and near despite prescription of proper spectacles. The best way to detect cataract is using a machine called the slit lamp bio-microscope. First the patient’s pupils are dilated. Next, the machine is used to examination of the anterior structures of the eye including the crystalline lens under magnification. The type and severity of the cataract and risk of developing cataract related complications such as lens-induced glaucoma is assessed. Attention is also paid to the clarity of the cornea and health of the retina, as diseases of these tissues will affect the successful outcome of cataract surgery.
8. How are cataracts treated?
The only treatment available for cataract is to replace the eye’s natural lens with an artificial lens. There are no eye drops, pills or diets that are proven in curing cataracts. Lasers too cannot be used to remove cataracts.
The principles of cataract surgery are simple. The cloudy lens is removed and replaced with an artificial intra-ocular lens implant made of biocompatible material such as acrylic, silicone or plastic materials. As every person’s eye power is different, the implanted lens has to be customized in terms of the lens power to neutralize most of any pre-existing refractive errors. This means that after cataract surgery, all patients can look forward to better vision without glasses!
9. When do I need to go for cataract surgery?
Cataract operation should be considered when vision impairment hampers the performance of daily activities such as reading, writing, driving, computer work and hobbies. In the early stages, some patients may find that a change in spectacles prescription may be all that is necessary to relieve the vision complaints. However, when this fails, cataract surgery is the only means to restore clear vision.
It is a myth that the cataract should be mature or “ripe” enough before surgery can be done. This commonly held folklore may have some truth when applied to the old way of doing cataract surgery but it no longer holds true with the advent of modern cataract surgery. On the contrary, earlier intervention is often recommended nowadays for earlier and faster visual rehabilitation and safer surgery.
Cataract surgery is one of the most commonly performed and safest operations with success rates of over 98% in the hands of a competent surgeon, and in the absence of other pre-existing eye diseases such as glaucoma, diabetic eye disease and retinal degeneration.
10. What does cataract surgery involve?
Modern cataract surgery is done as an outpatient procedure, meaning that no hospital stay is required. In the hands of a competent eye surgeon, it is a fast surgery done in 15 minutes without stitches and under just eye drops anaesthesia. As it is a delicate surgery done under magnification using an operating microscope and micro-surgical instruments. Patient co-operation is required – they should not move their heads unnecessarily or squeeze their eyes hard throughout the procedure. If the patient is unduly apprehensive or tense or unlikely to co-operate, then a regional block anaesthesia or general anaesthesia may be recommended.
Currently, there are two main types of cataract surgery. These are Phaco-emulsification Cataract Surgery and Extra-Capsular Cataract Extraction Surgery.